Change management case study
Improving the healing rates of venous leg ulceration using a pathway approach – 5 steps to successful change
1. Acknowledging and understanding the need for change
An audit undertaken across the community nursing teams had identified several concerns.
- Lack of holistic leg ulcer assessment
- Delays in obtaining or lack of ABPI
- Full/ therapeutic compression not routinely implemented
- High use of reduced compression
- High percentage of patients still unhealed after 12 months
Understanding the problem
I facilitated a focus group to discuss the audit findings and to gain some understanding as to why we found ourselves in this situation. The key themes that emerged from the focus group included:
- Lack of time
- Lack of confidence in decision making
- Poor clinical skills – no competency framework in place for Leg ulcer assessment/ management.
- Leg ulcers seen as less of a priority to other community nursing interventions
- Inconsistencies in clinical leadership
- No system in place for measuring outcomes (e.g healing rates)
- Delays in referring patient to Tissue viability
2. Communicating the change – involving the right people
I delivered a paper to the senior management team (including the Director for Community Services) that set out the audit and focus group findings. In addition, I had prepared some costings based on the time spent by community nurses on leg ulcer care for patients over a 12 month period and compared it to the potential costs if we healed patients by 24 weeks.
The savings were considerable – approx. £300K a year.
3. Develop change plans
Development of an evidence-based Venous leg ulcer treatment pathway based on 24-week healing.
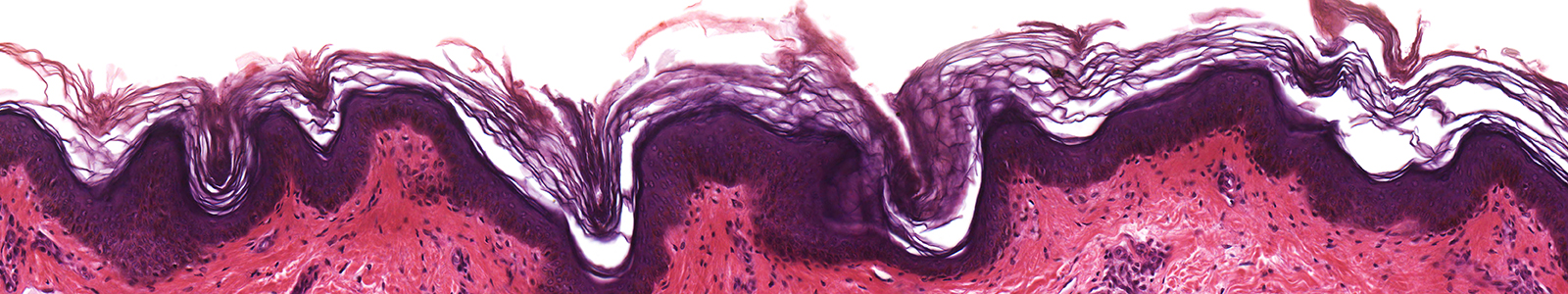
A Venous leg ulcer treatment pathway was created based on 6 weekly milestones that measured healing progress. There was an expectation that the ulcer should have achieved a 40% reduction in surface area every 6 weeks. If this was not being achieved this triggered a referral to Tissue Viability for advice. The pathway also focussed on wound cleaning/ debridement, the management of any local infection, management of elevated protease levels and the application of full compression. A target of 70% of patients with a VLU being healed at 24 weeks was set.
In addition to the pathway, a Patient Status At a Glance (PSAG) board was designed that set out the clinical activity expected from the community nurses pre and post implementation of the pathway. This included timeframes for undertaking assessment and ABPI.
Re-design of venous leg ulcer training programme
The existing leg ulcer training course was re-designed to incorporate the new pathway. It was extended to a 2-day course. Day 1 focussed on the theory behind leg ulceration and the fundamentals of assessment and management. Detail was given on how to apply the new treatment pathway. Day 2 was a practical session that allocated sufficient time for observing and practising Doppler (ABPI) and Compression bandaging. Our colleagues from Industry were a considerable help with facilitating these workshops.
Competency frameworks were developed to use alongside the training course with nurses self-assessing against the individual criteria and then agreeing a development plan with their line manager or mentor.
Development of a system for outcome measurement
An electronic database was created for capturing PSAG data/ healing outcomes.
Recruitment of Tissue Viability resource nurses
To support the new pathway, several Tissue Viability resource nurses were recruited from the community nursing teams. They were provided with additional training by the TV team to ensure they were fully competent in terms of knowledge and skills. This model enabled additional support for the community nursing teams as the pathway was being implemented.
4. Implementation of change plan
Eight implementation workshops were delivered throughout the county with an expectation that all nurses attend one of the sessions. The workshops included mandatory compression bandaging sessions. Each workshop was attended by a senior manager who reinforced the importance of making this change.
5. Evaluation of change plan and celebrating success
Data was evaluated after 24 weeks of implementation. A total of 71% of patients with a VLU had achieved full healing within 24 weeks, with many healing well before that date.
Community nursing time or clinical capacity had improved as patients were moved from an average of 5 visits a week to 1 or 2 before being discharged after healing.
Formal feedback from the nursing teams was positive, with 95% preferring to use the pathway approach to care and feeling more confident to practice. Increased job satisfaction and general morale across staff was also evident.
The success of this implementation was shared at board level.