About Sarah Gardner
 I have been a nurse for nearly 40 years with most of that time being spent in the community.
I have been a nurse for nearly 40 years with most of that time being spent in the community.
I recall the reaction of a hospital-based colleague when I told her I was applying to do my District Nurse training. She was incredulous, telling me it would be a waste of a good nurse, it would damage my career and referred to the community as the ‘elephants’ graveyard’.
Luckily, I ignored her advice and 30 years on, I look back on my community nursing career with much happiness and a sense of personal and professional satisfaction. The community is the heartbeat of the NHS and where most care should be delivered with both in reach and outreach from specialist services.
District nursing
I spent 18 years working within the District nursing service, initially as a Clinical Team Leader and latterly as a Community practice teacher and Clinical Development Lead. My experience has left me feeling privileged and humbled to have been allowed into the lives of those I cared for.
The role taught me much about the impact of illness and disability on peoples lives and the struggle many have accessing the right services. It exposed gaps and inequitable care, particularly for those unable to navigate health and social care systems, and it raised the importance of being advocates for our patients and providing a ‘voice’ for them.
The strength and resilience of people at lifes end will always remain with me as will the memories of those with life changing illnesses or disabilities having to come to terms with their limitations.
District nursing taught me the importance of listening, of needing to put yourself in your patient’s world to try and understand how they are feeling or why they are reacting or behaving in a certain way. It reinforced the importance of having empathy and compassion, qualities inherent in nursing but unfortunately are not always evident across the care sector. To me these are cornerstones of nursing.
This role reinforced the strength and value of working as a multi-disciplinary team and how good communication is pivotal to its success. Being able to share patient case stories or concerns at primary health care team meetings provided a collaborative platform for problem solving and ensured that the right services were involved at the right time. I have been fortunate to have worked with some truly inspirational people.
District nursing also taught me that we should always strive for high standards and quality care. Patients deserve evidence-based care that will achieve the outcomes set out in the plan discussed and agreed with them. As a team leader, educator and clinical development lead, my role was to be a role model and to inspire and support others to be great nurses. I faced challenges along the way, but this is inevitable when working in the rapidly changing landscape of the NHS. As they say, every challenge contains within it the potential for opportunity and growth.
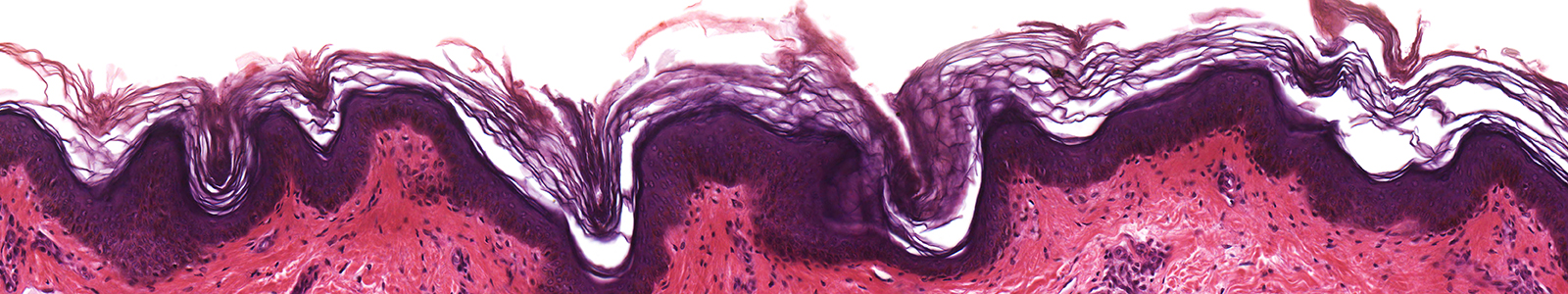
Up to 50% of a District Nurses caseload is spent on wound care, so my role provided me with ample opportunity to develop and ‘finely tune’ my knowledge and skills relating to this area of practice. The interest in Leg ulceration that stemmed from my dermatology years was reignited and I became the point of contact for my locality for providing advice and expertise on managing this condition. It was this interest in wound care that took my career in a new direction.
Tissue viability
I worked as clinical lead for Oxford Health, a community NHS Foundation Trust for 12 years. In that time I was able to demonstrate the value of having Tissue Viability specialists within the organisation and was able to expand and develop the team over the years.
The team supported a diverse number of services, all with their own individual needs. This included mental health services, community hospitals, District nursing, community childrens services and learning disability services. Externally we supported GP practices, Nursing homes and local hospices. In addition, the team provided an equipment service to those requiring pressure relieving equipment in the community.
My role was to provide clinical leadership to the Trust in terms of informing/ influencing decision making and strategy and I was able to this effectively because my feet were firmly planted in direct clinical practice. Im a great believer that respect for what you do has to be earned and demonstrated. To be a good clinical leader you must be exposed to the problems other nurses/ clinicians are dealing with. My high level of expertise was developed over many years. This tacit knowledge, which is sometimes difficult to describe, is formed through experience, reflection and education and the application of evidence-based practice that results in the outcomes you had been hoping for. Academically I studied to Masters level and kept myself up to date in terms of best evidence to inform my practice and advise on local policy and guidelines.
During my Tissue viability career I developed advanced clinical skills such as sharp debridement and advanced compression bandaging skills which enhanced my autonomy as a practitioner in terms of clinical decision making. As a predominantly nurse led service, it is essential that specialist nurses have the skills to independently assess, diagnose and treat patients without the need to refer on to other services for interventions that can easily be undertaken by themselves.
Through national networking and my role as Trustee for the Tissue Viability Society I have been fortunate to work as a Key Opinion Leader (KOL) on projects with various stakeholders. This has included being part of expert panels, contributing to consensus documents, presenting papers at conferences, and teaching more informally in small group sessions.
Although I am now working independently, my long NHS career puts me in a good position to work with NHS Trusts on developing strategies for improving wound care or avoiding unnecessary skin breakdown. I would also welcome opportunities to work with other stakeholders such as Industry, further education, the private sector and the voluntary sector.
Tissue Viability Society
I have been a Trustee for the TVS since 2016. The TVS is a charity whose mission is to disseminate information, promote research and increase awareness of all aspects of good clinical practice in wound prevention and management.
My role as Trustee is to help guide the strategic direction of the Society and this is achieved by my contribution at the Trustee meetings, effective decision making and my involvement in the projects that support the sub – groups such as Legs Matter.
A significant event in the TVS calendar is its conference. This annual event offers high quality, research-based education to clinicians, researchers and academics and provides a platform for sharing best practice through its symposiums or poster presentations. Trustees give their own time to support the smooth running of the conferences and will contribute as speakers, as chairperson to the symposiums and points of contact for both delegates and exhibitors. We also help man the TVS stand in the exhibition hall, talking to our existing members and encouraging new members. It is an exhausting but enjoyable few days and very rewarding knowing that the society has helped increase the knowledge and skills of so many people.
This conference would not be possible without the support from our colleagues in Industry who provide the generous educational grants that help fund delegate places.
Legs Matter
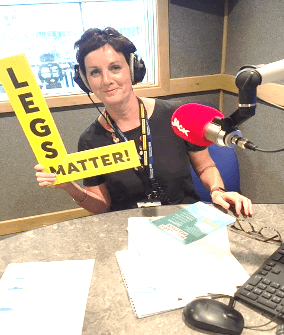
I have been part of the Legs Matter coalition (representing the Tissue Viability Society) since its inception in 2018 and feel very privileged to be working alongside such a fantastic group of people who are passionate about improving care for people with lower limb and foot problems. Legs Matter, governed by the Tissue Viability Society, is totally not for profit and has representation from the British Lymphology Society, Accelerate CIC, The Society of Vascular Nurses, FDUK, the College of Podiatry, the Leg Club Foundation and the Leg Ulcer Forum. We came together to campaign for better public awareness of lower limb and foot conditions and for improved care for those suffering with these conditions. We have a number of patient partners who sit equally alongside us as a coalition and who have shaped so much of our decision making due to sharing their personal experiences.
The Ongoing funding of our campaign has been achieved by generating sponsorship from our corporate partners. Working collaboratively with Industry has been really positive and their role is essential to help promote the objectives of the campaign.
Our website legsmatter.org has been a phenomenal success for us and has become an important platform for both patients and their family and friends as well as Health Care Professionals in accessing information about lower limb and foot conditions.
This year (2020) we have turned up the heat on our campaign to improve care for patients with leg and foot conditions and we are urging people to “Get Loud” and challenge the current status quo.
The 2020 awareness week has a patient/ public focus. We need people to be better informed and to challenge care that is not proving effective.
I truly believe there has been a significant shift in the lower limb ‘agenda’ and things will start to improve. NHS England’s National Wound Care Strategy Programme (NWCSP) includes a lower limb workstream which will shortly be rolling out evidence based guidance on managing lower limb and foot wounds and the implementation of the lower limb wound CQUIN (Insert number) will help address inconsistences of leg ulcer care by NHS community health providers.
Legs Matter will continue to provide an independent voice that will not be silenced until we are satisfied that patients get the care that they deserve.